The Shoulder

The shoulder is one of the most complex joints in the human body. What makes it remarkable is that it has minimal constraints, allowing us an incredible amount of motion. In fact, the shoulder is the most mobile joint in the human body. However, this motion also comes with a cost, as the very mechanisms that allow us so much motion also can be prone to injury.
If you’re experiencing shoulder pain, call one of our offices or book an appointment online to get started.
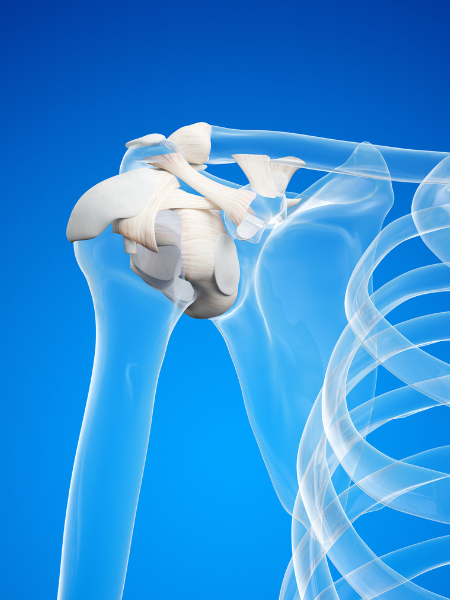
Shoulder Anatomy
The shoulder consists of one major joint called the glenohumeral joint and a smaller joint called the acromioclavicular joint, or AC joint. The glenohumeral joint is a loose ball and socket joint which is what allows most of the motion of the shoulder. The glenoid is the socket portion of the joint, but it is very shallow. This socket is deepened by a cartilage structure known as the labrum. The labrum is what is responsible for much of the stability in the shoulder.
The AC joint connects the clavicle and a portion of the shoulder blade called the acromion. It helps with a person’s ability to raise their arm up overhead. This joint is stabilized by 2 sets of ligaments, the acromioclavicular (AC) ligaments and the coracoclavicular (CC) ligaments.
A healthy functioning shoulder not only requires these joints to be in good condition, but also benefits from soft tissue support from muscles, ligaments, and tendons. The rotator cuff is one of the most important of these stabilizers in the shoulder. It is actually made up of 4 muscles all of which attach as tendons to the proximal humerus of the shoulder.

What causes
shoulder pain?
What causes shoulder pain?
There are many causes of shoulder pain. Some common ones can be damage to the cartilage of the shoulder leading to arthritis, tears of the labrum caused by shoulder dislocations, tears of the rotator cuff, or inflammation known as shoulder bursitis. Pain from these injuries can be experienced in various locations, including along the shoulder blade, at the front of the shoulder, or at the top of the shoulder depending on the cause of your symptoms.
Treatment
At Pacific Crest Orthopedics we customize a treatment plan to meet your individual needs. When it comes to the shoulder, some of the most common treatments can include different types of injections, use of anti-inflammatories, physical therapy, and use of a sling. For some conditions, surgery is indicated as the best option. See more on our surgery treatments.
Ephraim Dickinson, MD at Pacific Crest Orthopedics have extensive experience treating your shoulder pain and providing therapies to prevent future problems and to keep you active and healthy. Don’t continue to suffer from shoulder pain or immobility. If you have questions about shoulder pain, call Pacific Crest Orthopedics in San Francisco or use the online booking tool to schedule an appointment today.

Real Stories, Real Recovery.